URINARY SYSTEM
During the process of metabolism small particles of food and oxygen are rearranged into new forms. These are called waste products. When sugars and fats combine with oxygen in cells, they produce gases called carbondioxide and water vapor, which are removed from the body during respiration by lungs. When proteins combine with oxygen in cells they produce nitrogenous wastes which are difficult to be removed by respiration. These nitrogenous wastes are converted into urea in the liver. The urea is carried by blood stream to kidneys from where it is excreted in urine. Kidneys also produce a hormone called erythropoietin which helps in erythropoiesis. It also regulates the electrolytes (sodium, potassium, bicarbonate) in the body.
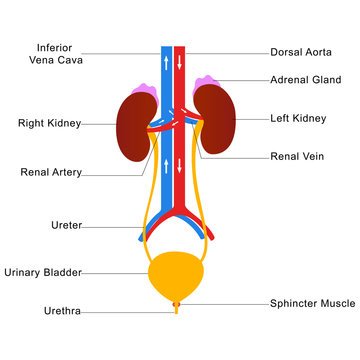
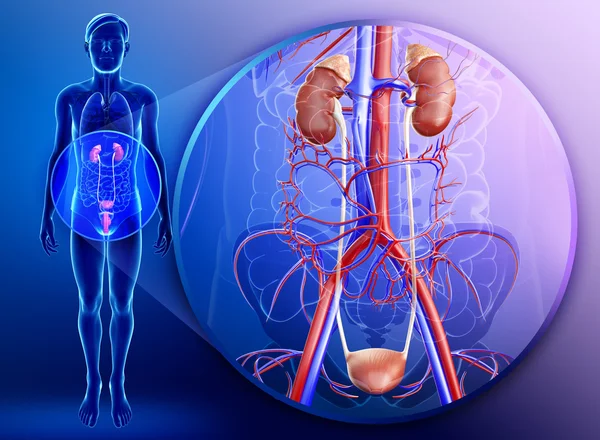
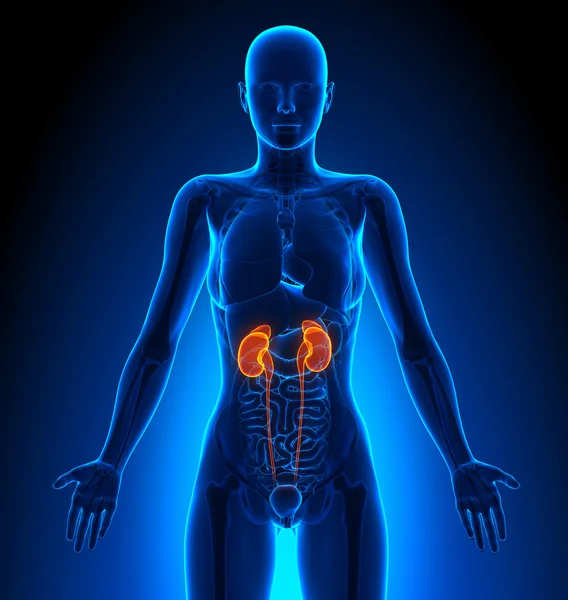
The urinary system is the main excretory system of the body. It consists
- Two kidneys.
- Two ureters.
- One urinary bladder.
- One urethra.
KIDNEY:
They are two bean-shaped organs lying on the posterior abdominal wall on each side of the vertebral column. The kidneys extend from the level of last thoracic vertebrae to the third lumbar vertebrae. The right kidney is smaller than the left kidney. The outer border of kidney is convex. The inner border is concave. Blood vessels enter and leave the kidney through the hilum. A suprarenal gland is situated at the apex of each kidney.
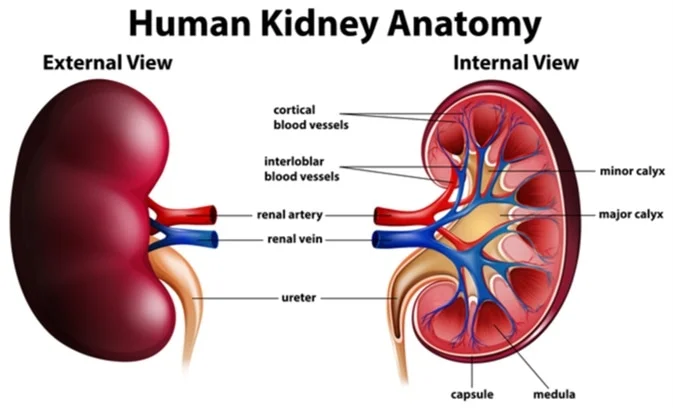
Structure: An outer fibrous capsule surrounds kidney, below this lies the substance of the kidney, which consists of:
- An outer cortex, which is reddish-brown in color.
- Inner medulla, which contains pyramids of the kidney.
- An upper expanded end of ureter called pelvis.
Microscopically the kidneys are made up of a number of structural and functional units called nephrons. There are about one million nephrons in each kidney. A nephron consists of two parts:
- Malphigian bodies made of Bowman’s capsule and glomerulus.
- Renal tubules.
The tubular part of the nephron is made up of:
- Proximal convoluted tubule situated in the cortex.
- Loop of enle present in the medulla. Henle present in the medulla
- Distal convoluted present in the cortex.
- Collecting tubules which pass through the medulla and open into the pelvis of kidney.
Blood enters into each kidney through the right and left renal arteries which branch into smaller arterioles which form a bunch known as glomerulus. The kidneys produce urine by a process called filtration. As blood passes through glomerulus salts, water, glucose , and urea are filtered and enter into the tubular part of the nephron. But only the wastes, some water, some salts remains in the renal tubules, the remaining material reabsorbed in the tubular part. Each renal tubule opens into collecting duct which in turn leads to renal pelvis. Renal pelvis continues below as ureter and drains into the bladder where urine is stored. At a later stage, after the bladder is filled up, it is excreted out by a process called micturition though urethra to the outside of the body.
URETER
It is a muscular tube which carries urine from the kidney to the bladder measuring about 26cm in length. It commences from the pelvis of the kidney, passes down in the abdominal cavity and opens in to urinary bladder.
URINARY BLADDER
It is a muscular sac which acts as a reservoir of urine. It lies in the pelvic cavity of the pubic symphysis.
The urinary bladder is a hollow, muscular, and distensible (or elastic) organ that sits on the pelvic floor in mammals. It is the organ that collects urine excreted by the kidneys prior to disposal by urination. Urine enters the bladder via the ureters and exits via the urethra.
In males, the bladder is superior to the prostate, and separated from the rectum by the rectovesical excavation.
In females, the bladder is separated from the rectum by the rectouterine excavation, and it is separated from the uterus by the vesicouterine excavation.
The triangular area between three openings is called trigone of the bladder.
URETHRA
It is a canal through which urine passes from bladder to the outside. It differs in males and females. But sphincter is present in both sexes. The external opening of the urethra is called urethral or urinary meatus.
MICTURITION
Urination, also known as micturition, voiding, and, more rarely, emiction, is the process of disposing urine from the urinary bladder through the urethra to the outside of the body. In healthy adults, the process of urination is under voluntary control; in infants and individuals with neurological injury, urination may occur as an involuntary reflex.
PATHOLOGICAL CONDITIONS
Dysuria : Difficulty or pain in urination.
Nocturia : Urination at night
Hematuria: Passing of red blood cells in urine.
Urgency: A strong desire of void accompanied by tear of leakage.
Pyuria: Presence of pus in urine
Oliguria: Scanty urine production.
Incontinence: Inability to prevent the discharge of urine.
Hesitancy: Delay/inability in starting urination.
Dribbling: To fall in drops
Renal failure:
Renal failure or kidney failure is a situation in which the kidneys fail to function adequately. It is divided in acute and chronic forms; either form may be due to a large number of other medical problems.
Biochemically, it is typically detected by an elevated serum creatinine. In the science of physiology, renal failure is described as a decrease in the glomerular filtration rate. When the kidneys malfunction, problems frequently encountered are abnormal fluid levels in the body, deranged acid levels, abnormal levels of potassium, calcium, phosphate, and (in the longer term) anemia. Long-term kidney problems have significant repercussions on other diseases, such as cardiovascular disease Stages of renal failure
- Diminished renal reserve
- Renal insufficiency
- Renal failure
- End-stage renal disease.
POLYCYSTIC KIDNEY DISEASE:
Polycystic Kidney Disease (also known as Polycystic Kidney Syndrome) (PKD) is a progressive, genetic disorder of the kidneys. It occurs in humans and other organisms. PKD is characterized by the presence of multiple cysts (hence, “polycystic”) in both kidneys. The disease can also damage the liver, pancreas, and rarely, the heart and brain.
GLOMERULONEPHRITIS
Glomerulonephritis is a type of kidney disease caused by inflammation of the internal kidney structures (glomeruli), which help filter waste and fluids from the blood.
Causes:
Glomerulonephritis may be caused by specific problems with the body’s immune system, but the precise cause of some cases is unknown. Damage to the glomeruli causes blood and protein to be lost in the urine.
The condition may develop after survival of the acute phase of rapidly progressive glomerulonephritis. In about a quarter of people with chronic glomerulonephritis there is no prior history of kidney disease and the disorder first appears as chronic renal failure.
URINARY TRACT INFECTION
A urinary tract infection (UTI) is a bacterial infection that affects any part of the urinary tract. Although urine contains a variety of fluids, salts, and waste products, it usually does not have bacteria in it. When bacteria get into the bladder or kidney and multiply in the urine, they cause a UTI. The most common type of UTI is a bladder infection which is also often called cystitis. Another kind of UTI is a kidney infection, known as pyelonephritis, and is much more serious. Although they cause discomfort, urinary tract infections are usually quickly and easily treated by seeing a doctor promptly.
PYELONEPHRITIS:
Acute pyelonephritis: Acute infection of the kidney caused by bacterial infection. Abscess (pus) formation is present in the renal pelvis.
Chronic pyelonephritis: Progressive damage caused by chronic infection leads to scarring of renal tissue, dilation and blunting of renal calyces. Treatment is by using broad spectrum antibiotics and work up for the cause.
RENAL HYPERTENTION:
Increase in blood pressure resulting from kidney disease. Renal artery stenosis results in 2- 5 % cases of renal hypertension because of increase in secretion of rennin (potent vasoconstrictor) by the involved kidney. Other causes of renal hypertension include glomerulonephritis and polycystic kidney. Treatment depends upon the causes.
Nephrolithiasis: The process of forming a kidney stone, a stone in the kidney (or lower down in the urinary tract).
Kidney stones are a common cause of blood in the urine and pain in the abdomen, flank, or groin.
Kidney stones occur in 1 in 20 people at some time in their life.
The development of the stones is related to decreased urine volume or increased excretion of stone-forming components such as calcium, oxalate, urate, cystine, xanthine, and phosphate. The stones form in the urine collecting area (the pelvis) of the kidney and may range in size from tiny to staghorn stones the size of the renal pelvis itself.
RENAL CELL CARCINOMA (HYPERNEPHROMA)
It is most common in between the ages of 60’s and 70’s. Clinical symptoms include hematuria and fever. Prognosis depends on tumor size and the extent of its spread at the time of diagnosis. Renal call carcinoma has a tendency to metastasize widely to lungs and bones before giving rise to symptoms. Treatment includes surgery and radiotherapy.
GOOD PASTURE SYNDROME
It is an acute immune disorder in which antibodies are present against the basement membrane of lung and kidney. Clinical features are hemoptysis and progressive renal failure. Treatment is by steroids.
NEPHROTIC SYNDROME
This condition is characterized by albuminuria, hypoalbuminemia accompanied by edema and hyperlipidemia. Etiology is idiopathic in majority of cases and in some it may be secondary to DM, SLE and drugs.
DIVERTICULA
Abnormal protrusion of mucosal membrane through a defect in muscle layer of bladder. They may arise as congenital defects but are mostly due to persistent outflow obstruction. Diverticula are the sites for urinary stasis and predispose to infection and stone formation.
ACUTE AND CHRONIC CYSTITIS
Large number of bacteria (such as E.coil, proteus and tuberculosis) fungus (Candida and Cryptococcus), worm (schistosoma) and sometimes radiation may also cause cystitis. Symptoms caused by cystitis include urinary frequency, lower abdominal pain and pain of burning on micturition.
CARCINOMA OF BLADDER
Bladder cancer characteristically causes blood in the urine; this may be visible to the naked eye (frank haematuria) or detectable only by microscope (microscopic haematuria). Other possible symptoms include pain during urination, frequent urination or feeling the need to urinate without results. These signs and symptoms are not specific to bladder cancer, and are also caused by non-cancerous conditions, including prostate infections and cystitis.
Based on cell type, it is divided into:
- Transitional (90%)
- Squamous (5%)
- Mixed (5%)
Risk factor includes industrial exposure to dyes, cigarette smoking, and analgesic abuse. Staging of the tumor is based on the depth of involvement of mucosa, bladder wall, and extent of metastases. Clinical symptoms include painless hematuria, frequency, urgency, and /or dysuria. Treatment is surgery (cystectomy), radiotherapy.
CLINICAL PROCEDURE & LABORATORY TESTS
Urinalysis:
- Color: Normal color of the urine is straw or yellowish. Variations in color of urine such as color less pale urine indicated larger amounts of water in urine smoky red colored appearance may be due to the presence of red cell casts, foods such as beetroots can produce red colored urine.
- pH : Normally the urine is slightly acidic. With infection the pH may be alkaline owing to the action of bacteria in urine, which convert urea to ammonia.
- Proteins: Normally minute amounts of proteins are present in urine which cannot be detected by ordinary laboratory procedure. Detection of large amount of proteins in the urine is usually because of damage to glomerular membrane. The majority of the protein excreted in urine is constituted by albumin.
- Glucose: Normally glucose that is filtered is reabsorbed completely. But in conditions where the blood glucose is higher than renal threshold (normal limit) the glucose cannot be reabsorbed which leads to passage of glucose in urine (glycosuria).
- Ketone: Ketones are breakdown products of fat metabolism. These bodies are usually absent in urine. Ketones are present in urine the conditions like diabetes mellitus, starvation.
- Specific gravity: It is the comparison of density of urine with the water. Normal specific gravity of urine is 1.010 – 1.020
- Cell counts: Normally 2-3 epithelial cells, 1-2 WBC are found in urine. In infections of the kidneys number of cells like WBC, RBC, pus cells and mucus cells can also be isolated.
Blood urea nitrogen (BUN): This test measures the amount of urea in the blood. Normally, kidneys excrete majority of the urea in urine. However, in the disease condition of kidneys the urea is not excreted and there will be increased levels of urea in the blood. This will be disproportionate amount of creatinine in the blood compared with the amount in the urine.
X-ray of Kidney, ureter and bladder (KUB): Plain radiography of the abdomen detects opaque calculi or calcification within the urinary tract. It also demonstrates the size and location of kidneys in relation to other organs.
Renal ultrasound: This is the choice of investigation for assessing renal size. It helps in distinguishing solid tumors from cysts. Renal tumors, hydronephrosis, polycystic kidney, dilation of renal pelvis and ureters, which indicate urinary tract obstruction can be screened. It is also used to access residual urine in the bladder after micturition.
Intravenous pyelography: Contrast materials injected intravenously, which travels to the kidney where it is filtered and excreted by glomeruli. It is used to demonstrate the size, shape and position of kidney and to study the outflow tract. Following injection, films are taken at timed intervals.
Voiding cystourethrography (VCUG): Using a catheter, bladder is filled with contrast medium and while the patient is voiding (expelling urine) x-rays are taken. This is used for assessment of disorders in bladder emptying and urethral abnormalities.
Cystoscopy: Visual examination of the bladder with the help of a cystoscope. Scope is passed through the urethra into the bladder. Cystoscopy allows direct visualization of bladder mucosa and ureteric orifices, stones, tumor and erosions of bladder mucosa.
Cystometry: Cystometry is a diagnostic procedure that provides measurable feedback about the function of the bladder. Specifically, cystometry provides information about the muscle function, mechanics, and nerve response of the bladder and urinary tract.
Kidney transplantation: A kidney transplant is a surgical procedure performed to replace a diseased kidney with a healthy kidney from another person. The kidney may come from a deceased organ donor or from a living donor. Family members or individuals who are unrelated but make a good match may be able to donate one of their kidneys. This type of transplant is called a living transplant. Individuals who donate a kidney can live healthy lives with the remaining kidney.
Renal arteriography: This is used to demonstrate the renal arterial system. It is helpful in the diagnosis of renal artery stenosis and arteriovenous malformation.
Renal biopsy: Biopsy of the kidney can be obtained at the time of surgery (open) or through the skin (closed). A small piece of tissue is send to the laboratory for (HPE) histopathological examination.
Lithotripsy: Lithotripsy is a noninvasive (the skin is not pierced) procedure used to treat kidney stones that are too large to pass through the urinary tract. Lithotripsy treats kidney stones by sending focused ultrasonic energy or shock waves directly to the stone first located with fluoroscopy (a type of x-ray “movie”) or ultrasound (high frequency sound waves). The shock waves break a large stone into smaller stones that will pass through the urinary system. Lithotripsy allows persons with certain types of stones in the urinary system to avoid an invasive surgical procedure for stone removal.
Dialysis: In conditions of renal failure the BUN levels are high. These waste materials are separate from blood stream artificially as the function of kidney is compromised. Two types of procedures used are:
- Hemodialysis: In this the patient’s blood is pumped to the artificial kidney (the dialyzer): this absorbs waste materials and send out dialyzed blood into the blood stream.
- Peritoneal dialysis: In this fluid is introduced into the peritoneal cavity, which allows transfer of waste materials from the blood stream into the fluid. Fluid (with wastes) is then removed with the help of a catheter.
DRUGS USED IN UROLOGY
Diuretics
- High efficacy diuretics: furosemide, bumetanide, piretanide, ethacrynic acid.
- Medium efficacy diuretics: chlorothiazide, hydrochlorothiazide, polythiazide, cyclopenthiazide, benzthiazide, hydroflumethiazide, bendroflumethiazide, chlorthalidone, metolazone, xipamide, indapamide.
- Weak or adjunctive diuretics: acetazolamide, ethoxaolamide, spironolactone, triameterene, amiloride, theophyline, mannitor, ammonium chloride, potassium citrate, potassium acetate.
ANTIDIURETICS
- Antidiuretic hormone (ADH, Vasioressub)
- Thiazide diuretics.
ABBREVIATIONS
ADH : Antidiuretic hormone: vasopressin
ARF : Acute renal failure
BUN : Blood urea nitrogen
CAPD : Continuous ambulatory peritoneal dialysis
Cath : Catheter, catheterization
Cl : Chloride
CRF : Chronic renal failure
Cysto : Cystoscopic examination
ESRD : End –stage renal disease
ESWL : Estracorporal shock wave lithotripsy
HCO3 : Bicarbonate
HD : Hemodialysis
IVP : Intravenous pyslogram
K+ : Potassium, an electrolyte
KUB : Kidney, ureter and bladder
Na+ : Sodium, an electrolyte
pH : Symbol for degree of acidity or alkalinity
RP : Symbol for degree of acidity or alkalinity
TURP : Transurethral resection of the prostate
UA : Urinalysis
UTI : Urinary tract infection
VCUG : Voiding cystourethrogram